How Monitoring Real-time Air Quality Can Help Combat Viruses
The air we breathe, especially indoors, plays a crucial role in the spread and survival of viruses like COVID-19. Studies have shown that poor ventilation and inadequate air quality contribute to increased viral transmission, highlighting the need for proactive solutions. This is where real-time air quality monitoring devices like HibouAir step in, empowering us to understand and take control of our indoor air environments.
Understanding the Link Between Air Quality and Virus Transmission:
Viruses, including COVID-19, can spread through airborne transmission. When infected individuals cough, sneeze, or even talk, microscopic viral particles are expelled into the air. These particles can linger for extended periods in poorly ventilated spaces, increasing the risk of infection for others. Additionally, poor air quality, often characterized by high levels of pollutants and low humidity, can weaken our immune systems and make us more susceptible to viral infections.
Viruses and Bacteria: Invisible Threats in the Air
The air we breathe is not always as clean as we think. It can be teeming with invisible threats in the form of viruses and bacteria. These microscopic organisms can survive and spread in the air, posing a risk to our health.
How Viruses and Bacteria Spread in the Air:
Respiratory droplets: When an infected person coughs, sneezes, or talks, they release tiny droplets containing viruses or bacteria. These droplets can evaporate quickly, leaving behind even smaller particles known as droplet nuclei. These nuclei can remain suspended in the air for extended periods and travel long distances, potentially infecting others who inhale them.
Dust and aerosols: Viruses and bacteria can also attach to dust particles and other airborne contaminants. These contaminated particles can then be inhaled or deposited on surfaces, where they can remain viable for hours or even days.
Direct contact: Some viruses and bacteria can be transmitted through direct contact with contaminated surfaces and then touching your face.
Poor Ventilation and Air Exchange: A recipe for virus spread in closed spaces
The air we breathe indoors plays a crucial role in our health and well-being. However, poor ventilation and inadequate air exchange in closed spaces can create a breeding ground for viruses, significantly increasing the risk of their spread.
Several studies have demonstrated the link between poor ventilation and increased virus transmission:
A study published in the journal “Indoor Air” found that the risk of tuberculosis transmission was four times higher in poorly ventilated rooms compared to well-ventilated rooms. A study published in the journal “The Lancet” found that the risk of influenza transmission was three times higher in poorly ventilated classrooms compared to well-ventilated classrooms. A study published in the journal “Emerging Infectious Diseases” found that the risk of COVID-19 transmission was 19 times higher in poorly ventilated restaurants compared to well-ventilated restaurants.

A group of colleagues meets in a poorly ventilated work space for a long time. One person is infected with a virus and unknowingly coughs, releasing virus particles into the air.
Many students gather in a classroom with limited air circulation for several hours. One student has a cold and spreads the virus through coughing and sneezing.

Open windows, utilize air purifiers, monitor air quality with HibouAir, limit meeting duration, and encourage mask-wearing would help mitigate these issue.
Components of Air Quality and Their Impact on Virus Survival in Closed Spaces
Several key components of air quality play a crucial role in the survival and transmission of viruses in closed spaces. Understanding these factors is essential for taking proactive measures to create safer and healthier environments.
Temperature: Generally, viruses survive better at cooler temperatures, typically between 40°F and 60°F. However, some viruses, like the flu virus, can survive at warmer temperatures as well. While cold temperatures may initially slow down viral activity, they do not necessarily kill the virus. When temperatures rise again, the virus can become active once more.
CO2: While not directly affecting virus survival, elevated CO2 levels in poorly ventilated spaces can indirectly increase the risk of transmission. This is because high CO2 levels can lead to increased breathing rates and deeper breaths, potentially increasing the amount of virus inhaled.

Particulate Matter (PM1.0, PM2.5, PM10): These tiny particles can act as carriers for viruses, providing a surface for them to attach and remain airborne for longer periods. This can potentially increase the risk of transmission, especially in poorly ventilated spaces.
Humidity: Studies suggest that high humidity levels (above 60%) may slightly increase the survival time of certain viruses in the air. However, the impact of humidity varies depending on the specific virus and other environmental factors. Dry air can damage the outer layer of some viruses, potentially reducing their infectivity. However, low humidity can also irritate the respiratory tract, making people more susceptible to infection.
Air Pressure: While not directly impacting virus survival itself, air pressure can influence ventilation rates in enclosed spaces. Higher air pressure can trap pollutants and viruses inside, while lower pressure can facilitate better air exchange and reduce virus concentration.
HibouAir’s Virus Index: A Powerful Tool to Combat Virus Transmission
The global pandemic has highlighted the critical need for solutions that help us understand and mitigate the risk of viral transmission. Recognizing this need, HiBouAir has developed a revolutionary feature called the Virus Index. This AI-powered tool provides real-time insights into the risk of virus spread in closed environments, empowering individuals and organizations to make informed decisions for a safer and healthier world.
How does the Virus Index work?
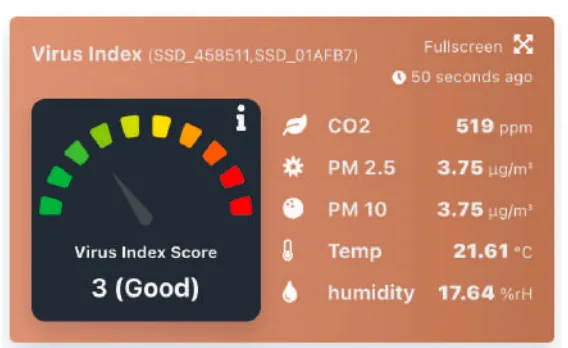
The Virus Index analyzes various air quality parameters, including temperature, humidity, CO2 levels, and particulate matter (PM), in real-time. This data is then fed into a sophisticated AI algorithm that assesses the combined impact of these factors on the viability and transmission of viruses like COVID-19.
Virus Index Range and Interpretation:
The Virus Index displays a score ranging from 1 to 10, categorized into four distinct levels:

Benefits of the Virus Index:
Real-time risk assessment: Provides immediate insights into the risk of virus spread, allowing for proactive intervention.
Data-driven decision making: Guides the implementation of appropriate safety measures based on real-time data analysis.
Increased peace of mind: Empowers individuals and organizations to take control of their health and safety in closed spaces.
Early warning system:
Alerts users to potential risks before they escalate, allowing for timely mitigation strategies.
Improved preparedness: Helps prepare for future pandemic outbreaks by providing valuable data and insights.

HibouAir’s Virus Index is a game-changer in the fight against viral transmission. By providing real-time insights into the risk of infection, this innovative technology empowers individuals and organizations to create safer and healthier environments for everyone. With HiBouAir, we can move towards a future where viruses no longer pose a significant threat to our health and well-being.
References:
– Centers for Disease Control and Prevention:
https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/overview/index.html
– National Institutes of Health:
https://en.wikipedia.org/wiki/Airborne_transmission
– Emerging Infectious Diseases (2020) High attack rate of COVID-19 among restaurant patrons during infectious period of source person
https://www.cdc.gov/mmwr/volumes/69/wr/mm6936a5.htm
– World Health Organization. (2020, March 30). Ventilation and air conditioning in public spaces and buildings. https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-ventilation-and-air-conditioning-in-public-spaces-and-buildings
– Centers for Disease Control and Prevention. (2022, July 8). Ventilation in buildings. https://www.cdc.gov/coronavirus/2019-ncov/community/ventilation.html
– The Lancet. (2012). Respiratory viral infections in classrooms and the role of ventilation: A school intervention study. https://pubmed.ncbi.nlm.nih.gov/20816549/
– Harvard Health. (2022, November 1). Easy ways you can improve indoor air quality. https://www.ehs.harvard.edu/programs/indoor-air-quality-iaq
– Indoor Air. (2004). Risk of tuberculosis transmission in relation to ventilation in healthcare settings. https://pubmed.ncbi.nlm.nih.gov/11085840/
– Healthline. (2022, February 15). How to Improve Air Quality at Home: 8 Tips to Try. https://www.healthline.com/health/how-to-improve-air-quality-at-home
– US Environmental Protection Agency. (2023, July 27). Improving Indoor Air Quality. https://www.epa.gov/indoor-air-quality-iaq